What is orthobiological treatment?
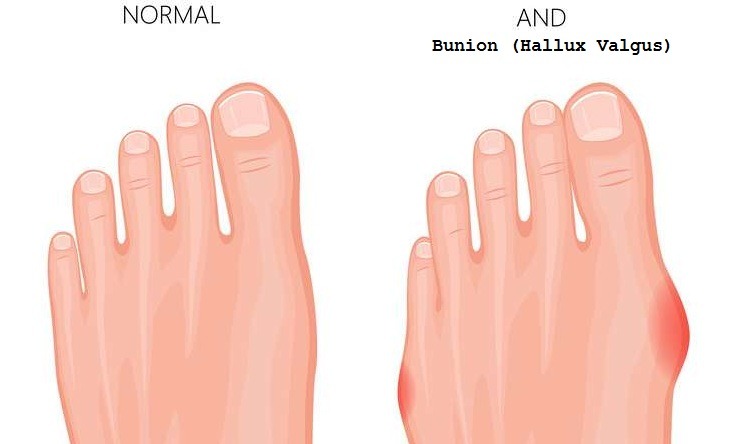
Orthobiological treatments are among the most discussed and interesting topics of recent times. They are deemed as treatment supportive methods, which are believed to help repair and prevent the wear and tear of tendons, cartilages, meniscus and ligaments, bones. Orthobiological applications carried out for this purpose can be listed as; Hyaluronic Acid injections can be listed as PRP and stem cell applications and cord or embryonic cell treatments. These orthobiological methods can be used alone or to support recovery after a surgical treatment.
HYALURONIC ACID INJECTION
While hyaluronic acid is not a biological agent, it is useful in the treatment process with its application into the joint. It shows its effect by lubricating the bone and cartilage surfaces in the joint and reducing wear due to friction. It reduces edema and pain. There are various forms of hyaluronic acid as low, medium and high molecular weight. Recently, a single long-acting double-chain injection application replaced the three sequential dose application.
In our experience is Hyaluronic acid; is beneficial in moderate cartilage abrasions together with physical therapy applied after injection. We obtain good results by combining with isokinetic physical therapy in the treatment of knee cap cartilage deformities that cause anterior knee pain. Even through it is not generally beneficial in advanced calcification (osteoarthritis), we observe that when it works, it is effective in a short time. We try to reduce the pain with cortisone injections instead of hyaluronic acid in our patients with advanced calcification (osteoarthritis) who do not want to undergo surgical treatment or cannot be operated due to other accompanying diseases.
ORTHOBIOLOGICAL PRP (PLASMA ENRICHED FROM COAGULATION CELLS)
Orthobiological PRP application is obtained by centrifuging the patient’s own blood and separating it from red and sometimes white blood cells. Coagulation cells are high in concentration in the portion obtained after centrifugation. It activates a mechanism similar to wound healing in the area it is applied to with the help of coagulation cells and some tissue healing substances. The benefit of PRP, which is an orthobiological application, is that these tissue-healing cells and substances can be concentrated and injected to the damaged area. It is believed to aid in the treatment of intra-knee cartilage and ligament injuries, tendon problems such as tennis elbow and Achilles tendinitis.
In our clinic, we apply PRP mostly to support tissue healing in the post-arthroscopic period, meaning after closed knee surgeries. We use closed system PRP kits (Arhrex), which we believe minimize the risk of infection and which can be applied with a single injector. We apply the injections 3 times with an interval of 20 days. If we are performing it after surgery, we will make the first injection 1 month after surgery. In moderate knee cartilage disorders, we perform PRP and hyaluronic acid injections consecutively. Thus, we benefit from both the healing effect of PRP and the lubricating effect of hyaluronic acid.
PRP has replaced cortisone injections in lateral epicondylitis disease called tennis elbow. It is claimed that the need for surgical treatment decreases with 1 or 2 sessions of PRP applied in the middle period of the disease becoming chronic (1-6 months). In our clinic, we were able to provide healing in approximately 60% of our patients who got PRP injections for the diagnosis of tennis elbow. The injection to be made exactly at the target point and cortisone not being applied previously were factors that increased our achievement of good results in our patients who applied to us with tennis elbow disease.
The results of PPR application in the shoulder joint have been reported negatively in many scientific studies. Although it is advocated in some scientific circles that it may increase healing after arthroscopic shoulder tendon rupture repair, we do not use PRP injections for the treatment of shoulder joint diseases in our routine practices.
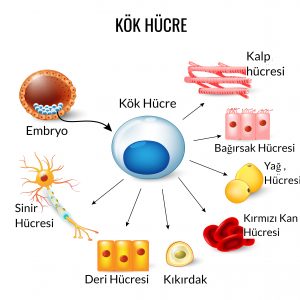
ORTHOBIOLOGICAL STEM CELL APPLICATIONS
It helps the repair activity by transforming into the main cells of the tissue to which they are applied. It can be applied by deriving from bone marrow and adipose tissue. Stem cells originating from adipose tissue bear the same characteristics as those originating from bone marrow. Depending on the area of application, they can turn into bone, cartilage, muscle, and adipose tissue and enable the release of enzymes and growth factors that will trigger production repair activities. The advantages over bone marrow-sourced delivery systems are that it is easier to take and the number of cells is higher due to the larger donor tissue. It is generally applied in arthroscopic cartilage, ligament and meniscus surgeries or intra-bone pressure reduction surgeries for bone edema to support cell regeneration in the cleaned area.
Advantages of Adipose Tissue Sourced Stem Cell Application
- It regulates the formation of edema.
- It protects against the tissue from hardening called fibrosis.
- It resists cell aging and death.
- It provides tissue regeneration by supporting vascularity.
- It reduces joint calcification (osteoarthritis) and swelling called osteophytes.
- It reduces cartilage wear.
- It helps to complete the scantiness or production deficiency of the tissue’s own stem cells.
Click for detailed information about stem cell applications!